Agency: Health Line Item: Health Care Financing Function The Division of Health Care Financing is the administrative agency for Utah's Medical Assistance Programs (Medicaid, Children's Health Insurance Program, Utah's Premium Partnership for Health Insurance, and Primary Care Network). As per federal requirements, all funding for Medicaid must flow through the Department of Health and be governed by a memorandum of understanding for all functions performed by other entities whether State, non-profit, for profit, local government, etc. About 83% of the medical services are provided by any willing provider who bills Medicaid directly. The other 17% of medical services are provided through two contracted health plans who handle the billing and case management services of their clients.
Federal regulations provide for a wide variety of funding ratios ranging from 50 to 90 percent for different classes of positions and functions for this Division. The Division includes the following seven offices or bureaus: Director's Office, Financial Services, Eligibility Policy, Coverage and Reimbursement, Medicaid Operations, Managed Health Care, and Long-term Care. The Division also includes the following three budget programs: DWS Seeded Services, Other Seeded Services, and Contracts. Federal law requires that the Medical Care Advisory Committee serve as an advisory board to the Division. This committee consists of providers, Medicaid recipients, representatives from the Department of Human Services and the Department of Workforce Services, and members of the community. The committee advises the Division on program content, policy, and priorities. The Committee is advisory and its decisions are not binding on the Division. Medicaid Fraud Control Unit The Medicaid Fraud Control Unit's mission is: 'To protect the integrity of the Medicaid program and the safety and property of institutionalized citizens of the State of Utah through skilled detection, proactive investigation, prevention, prosecution and financial recovery.' The Unit operates in the Attorney General's Office and focuses on criminal and civil actions against fraudulent providers and perpetrators of neglect and abuse against vulnerable adults in care facilities. Statutory Authority The Division of Health Care Financing is governed by several chapters of the Utah Health Code in Title 26 of the Utah Code. - UCA 26-18 establishes the Medical Assistance Program, commonly referred to as Medicaid and its administrative arm, the Division of Health Care Financing.
- UCA 26-18-2.2 requires that the Medicaid director by appointed by the Governor with the consent of the Senate.
- UCA 26-18-402 establishes the Medicaid Restricted Account from unexpended General Funds. These funds may be appropriated by the Legislature for expanding medical assistance coverage.
- UCA 26-19 authorizes the Health Department to recover Medicaid benefits paid by the Division from third parties, including estates and trusts.
- UCA 26-20 prohibits false Medicaid claims and establishes the Medicaid Fraud Control Unit.
- UCA 26-35a creates the Nursing Care Facilities Account and levies an assessment on the owners of nursing care facilities to generate seed money which draws down additional federal funds for the reimbursement to those facilities.
- UCA 26-47 requires the Department to create a Prescription Drug Assistance Program to assist individuals who need help in obtaining prescription drugs at a reduced cost or at no cost.
- UCA 67-5-1 details the responsibilities of the Attorney General to investigate and prosecute abuse and neglect
Intent Language Under Section 63J-1-603 of the Utah Code the Legislature intends that appropriations provided for Health Care Financing in Item 101 of Chapter 2 Laws of Utah 2010 not lapse at the close of Fiscal Year 2011. The use of any nonlapsing funds is limited to $50,000 for the purchase of computer equipment. The Legislature intends that the Department of Health provide a report to the Office of the Legislative Fiscal Analyst by December 1, 2011 on the status of implementing recommendations from the following audits: (1) A Performance Audit of Utah Medicaid Provider Cost Control and (2) A Follow-up of Utah's Medicaid Implementation of Audit Recommendations. The items to be followed up on would be less to the extent that an Independent Medicaid Inspector General is established and takes over the responsibility for implementation of some recommendations. The report would not be needed if a follow up audit is prioritized for the Legislative Auditor General by July 1, 2011. The Legislature intends that the Department of Health report by October 1, 2011 to the Office of the Legislative Fiscal Analyst on reimbursement alternatives for inpatient hospital outlier payments that would give the State more control over inflationary increases and/or move away from a reimbursement based on billed charges. The report also shall explain the measures the Department takes to verify the validity of outlier claims. This report should include a report on any other reimbursements based on billed charges that totaled over $1,000,000 total funds in FY 2011 and options for moving away from paying as a percentage of billed charges. The Legislature intends that if SB 180 Medicaid Reform passes, the Department of Health shall issue requests for information and report back a summary of the results to the Office of the Legislative Fiscal Analyst by four months prior to providing services via new contracts. Funding Detail For analysis of current budget requests and discussion of issues related to this budget click here. | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $4,990,800 | $4,985,000 | $4,605,000 | $3,792,000 | $3,791,100 | | General Fund, One-time | $270,500 | ($84,600) | ($353,300) | $1,067,000 | ($60,100) | | Federal Funds | $64,437,400 | $63,158,900 | $54,212,000 | $55,062,600 | $55,099,900 | | American Recovery and Reinvestment Act | $0 | $111,300 | $158,900 | $184,200 | $0 | | Dedicated Credits Revenue | $6,050,200 | $4,935,700 | $2,242,900 | $9,720,900 | $2,263,500 | | GFR - Medicaid Restricted | $1,000,000 | $0 | $0 | $0 | $0 | | GFR - Nursing Care Facilities Account | $350,000 | $350,000 | $350,000 | $547,200 | $585,200 | | Transfers | $0 | $333,300 | $0 | $0 | $0 | | Transfers - Intergovernmental | $0 | $1,111,300 | $1,330,700 | $0 | $1,231,000 | | Transfers - Medicaid | $1,940,100 | $0 | $0 | $0 | $0 | | Transfers - Medicaid - DHS | $89,600 | $9,873,500 | $8,910,000 | $8,958,100 | $11,099,700 | | Transfers - Medicaid - DWS | $2,140,200 | $25,641,500 | $26,589,100 | $20,648,200 | $23,616,500 | | Transfers - Medicaid - Internal DOH | $0 | $0 | $0 | $1,395,200 | $0 | | Transfers - Medicaid - USDB | $0 | $0 | $0 | $25,900 | $0 | | Transfers - Other Agencies | $7,664,700 | $0 | $0 | $0 | $0 | | Transfers - Within Agency | $29,259,300 | $4,047,200 | $2,260,500 | $2,467,200 | $1,935,500 | | Beginning Nonlapsing | $0 | $750,000 | $493,600 | $492,300 | $0 | | Closing Nonlapsing | ($750,000) | ($493,600) | ($492,300) | ($40,400) | $0 | | Lapsing Balance | ($147,400) | $0 | $0 | $0 | $0 | | Total | $117,295,400 | $114,719,500 | $100,307,100 | $104,320,400 | $99,562,300 |
|---|
| | Programs: | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Director's Office | $2,964,700 | $3,035,300 | $2,871,100 | $2,580,500 | $2,552,300 | | Financial Services | $9,463,000 | $10,324,100 | $9,504,800 | $9,223,700 | $12,036,900 | | Medicaid Operations | $3,753,500 | $3,775,300 | $3,825,000 | $4,521,000 | $4,170,700 | | Managed Health Care | $3,416,900 | $3,693,800 | $3,418,000 | $3,132,300 | $3,206,400 | | Long-term Care | $1,851,500 | $2,035,700 | $2,464,800 | $2,955,200 | $2,474,700 | | Contracts | $81,170,900 | $76,523,800 | $67,907,700 | $13,854,100 | $2,240,200 | | Coverage and Reimbursement | $5,992,600 | $3,184,000 | $2,360,900 | $1,863,300 | $2,047,700 | | Eligibility Policy | $8,681,500 | $10,015,200 | $6,449,000 | $2,217,000 | $1,669,900 | | Department of Workforce Services' Seeded Services | $0 | $0 | $0 | $41,356,200 | $47,164,600 | | Other Seeded Services | $0 | $0 | $0 | $22,617,100 | $22,004,200 | | Program Integrity | $800 | $2,132,300 | $1,505,800 | $0 | ($5,300) | | Total | $117,295,400 | $114,719,500 | $100,307,100 | $104,320,400 | $99,562,300 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $16,887,200 | $17,434,300 | $16,255,000 | $13,815,800 | $13,238,600 | | In-state Travel | $73,500 | $69,500 | $32,000 | $20,200 | $26,600 | | Out-of-state Travel | $51,400 | $70,600 | $14,600 | $21,500 | $12,500 | | Current Expense | $8,691,400 | $8,030,700 | $6,338,500 | $4,202,400 | $9,610,700 | | DP Current Expense | $7,891,200 | $7,790,200 | $7,588,900 | $7,483,200 | $7,280,000 | | DP Capital Outlay | $0 | $0 | $0 | $834,700 | $0 | | Other Charges/Pass Thru | $83,700,700 | $81,324,200 | $70,078,100 | $77,942,600 | $69,393,900 | | Total | $117,295,400 | $114,719,500 | $100,307,100 | $104,320,400 | $99,562,300 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 229.4 | 224.1 | 231.6 | 199.4 | 193.9 | | Actual FTE | 220.1 | 224.5 | 218.0 | 182.5 | 0.0 | | Vehicles | 3 | 3 | 3 | 3 | 3 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Director's Office Function The Director's Office of the Division of Health Care Financing administers and coordinates Utah's Medicaid Program and Children's Health Insurance Program to comply with Titles XIX and XXI of the Social Security Act, other laws of the State, and the appropriated budget. The Medicaid director is appointed by the Governor with the consent of the Senate. Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $320,200 | $122,300 | $288,400 | $323,600 | $78,200 | | General Fund, One-time | $63,500 | $165,400 | ($237,200) | ($274,200) | $0 | | Federal Funds | $1,739,100 | $1,772,900 | $1,931,900 | $1,346,800 | $1,662,400 | | Dedicated Credits Revenue | $1,433,500 | $1,747,100 | $1,715,600 | $2,928,700 | $1,715,600 | | Transfers - Intergovernmental | $0 | $987,300 | $1,330,700 | $0 | $1,231,000 | | Transfers - Medicaid | $1,940,100 | $0 | $0 | $0 | $0 | | Transfers - Medicaid - DHS | $89,600 | $363,500 | $465,900 | $169,000 | $431,000 | | Transfers - Medicaid - DWS | $0 | $0 | $37,000 | $88,400 | $34,200 | | Transfers - Within Agency | ($2,483,000) | ($2,079,600) | ($2,662,500) | ($2,453,700) | ($2,600,100) | | Beginning Nonlapsing | $0 | $0 | $493,600 | $492,300 | $0 | | Closing Nonlapsing | $0 | ($43,600) | ($492,300) | ($40,400) | $0 | | Lapsing Balance | ($138,300) | $0 | $0 | $0 | $0 | | Total | $2,964,700 | $3,035,300 | $2,871,100 | $2,580,500 | $2,552,300 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $1,302,900 | $1,219,500 | $1,083,400 | $1,135,900 | $797,100 | | In-state Travel | $6,500 | $1,800 | $4,600 | $4,100 | $4,500 | | Out-of-state Travel | $17,000 | $2,700 | $6,000 | $6,700 | $7,500 | | Current Expense | $534,900 | $582,300 | $501,800 | $264,900 | $467,100 | | DP Current Expense | $1,096,500 | $940,300 | $1,247,800 | $1,053,600 | $1,248,600 | | Other Charges/Pass Thru | $6,900 | $288,700 | $27,500 | $115,300 | $27,500 | | Total | $2,964,700 | $3,035,300 | $2,871,100 | $2,580,500 | $2,552,300 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 38.9 | 29.9 | 26.3 | 12.5 | 9.0 | | Actual FTE | 35.2 | 29.9 | 14.0 | 11.1 | 0.0 | | Vehicles | 0 | 0 | 3 | 3 | 2 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Financial Services Function The Bureau of Financial Services is responsible for the following functions within the Division: - Managing the administration and service budgets for Medicaid, Utah's Premium Partnership for Health Insurance, Primary Care Network programs, and the Children's Health Insurance Program.
- Monitoring, tracking, invoicing, and collecting drug rebates due from pharmaceutical manufacturers.
- Purchasing office equipment, computer hardware, and software for the Division.
- Managing contracts for the Division.
- Performing budget neutrality calculations on contracted health plans and comparing results to fee-for-service payments.
- Overseeing the collection of money from provider assessments.
- Performing Upper Payment Limit calculations for managed care plans.
- Preparing reports for the Centers for Medicare and Medicaid.
- Monitoring, tracking, invoicing, and collecting the Nursing Home and Hospital provider assessments.
- Projecting and forecasting the Medicaid budget.
- Monitoring, tracking, invoicing, and collecting seed revenue from other governmental entities.
Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $1,225,600 | $441,500 | $742,400 | $549,100 | $22,000 | | General Fund, One-time | $0 | $0 | ($78,400) | $0 | $0 | | Federal Funds | $6,146,500 | $7,329,000 | $6,290,800 | $6,190,400 | $9,429,700 | | American Recovery and Reinvestment Act | $0 | $0 | $0 | $184,200 | $0 | | GFR - Medicaid Restricted | $1,000,000 | $0 | $0 | $0 | $0 | | GFR - Nursing Care Facilities Account | $350,000 | $350,000 | $350,000 | $0 | $585,200 | | Transfers - Within Agency | $1,500,000 | $1,903,600 | $2,200,000 | $2,300,000 | $2,000,000 | | Beginning Nonlapsing | $0 | $750,000 | $0 | $0 | $0 | | Closing Nonlapsing | ($750,000) | ($450,000) | $0 | $0 | $0 | | Lapsing Balance | ($9,100) | $0 | $0 | $0 | $0 | | Total | $9,463,000 | $10,324,100 | $9,504,800 | $9,223,700 | $12,036,900 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $2,109,700 | $2,344,300 | $2,195,000 | $1,541,000 | $1,021,400 | | In-state Travel | $16,000 | $28,200 | $5,000 | $700 | $0 | | Out-of-state Travel | $5,400 | $46,000 | $4,000 | $7,100 | $0 | | Current Expense | $1,067,200 | $1,419,300 | $1,284,500 | $742,100 | $5,302,200 | | DP Current Expense | $6,264,700 | $6,486,300 | $6,016,300 | $6,098,100 | $5,713,300 | | DP Capital Outlay | $0 | $0 | $0 | $834,700 | $0 | | Total | $9,463,000 | $10,324,100 | $9,504,800 | $9,223,700 | $12,036,900 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 23.0 | 26.0 | 27.5 | 24.9 | 17.0 | | Actual FTE | 24.2 | 26.1 | 24.0 | 19.5 | 0.0 | | Vehicles | 1 | 1 | 0 | 0 | 1 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Medicaid Operations Function The Bureau of Medicaid Operations has the following five components: - Customer Service - The Bureau staffs the Medicaid Information Line, providing online service to providers and clients regarding Medicaid eligibility, provider payment, and general information regarding all aspects of services provided by Medicaid. An automated call management system ensures that calls get routed to the correct area without having to go through numerous transfers. There is an automated phone system for providers to verify client eligibility.
- Utah Health Information Network (UHIN) Involvement - UHIN is a statewide cooperative of Medicaid, providers, and other third party payers. Its goal is to standardize health care information so that all claims data can be submitted in an electronic transaction to participating payers.
- Medicaid Management Information System (MMIS) - Bureau staff identifies and approves updates and modifications to the MMIS to ensure the system is properly handling information on services provided by Medicaid. The staff also requests additional programming to implement policy changes and new federal/State regulations affecting claims processing. Staff is responsible for maintenance and data input of the MMIS subsystems, i.e. provider file, reference file, and security information.
- Claims Processing - The Bureau processes all claims received by Medicaid, ensuring that the claims are properly entered into the MMIS system, and are paid properly. The Bureau troubleshoots with providers in the event there are questions regarding payment or non-payment of claims, and coordinates repayment processes with other State and federal agencies. The majority of all claims are processed and paid electronically.
- Special Programs - The Bureau manages special programs under contract with Family Health and Preparedness (Prenatal program) and the Division of Child and Family Services (Custody Medical Care Program for foster care children). It also manages the Buy-out Program that ensures compliance with the third party liability requirements of the 1990 federal Omnibus Budget Reconciliation Act legislation. Additionally, the Bureau manages Utah Medicaid's required participation in the Indian Health Services federally-funded program.
Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $559,600 | $713,000 | $439,800 | $360,200 | $720,700 | | General Fund, One-time | $0 | ($250,000) | ($7,700) | $1,341,200 | ($60,100) | | Federal Funds | $2,693,900 | $2,706,000 | $2,653,800 | $2,519,600 | $2,719,000 | | Dedicated Credits Revenue | $0 | $0 | $0 | $0 | $12,000 | | Transfers - Medicaid - DHS | $0 | $37,500 | $39,100 | $0 | $0 | | Transfers - Within Agency | $500,000 | $568,800 | $700,000 | $300,000 | $779,100 | | Total | $3,753,500 | $3,775,300 | $3,825,000 | $4,521,000 | $4,170,700 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $2,964,700 | $3,132,100 | $3,065,900 | $2,846,100 | $3,372,300 | | In-state Travel | $4,400 | $5,700 | $5,300 | $5,200 | $5,300 | | Out-of-state Travel | $4,700 | $0 | $0 | $200 | $0 | | Current Expense | $520,400 | $420,000 | $528,100 | $501,900 | $567,500 | | DP Current Expense | $259,300 | $217,500 | $225,700 | $221,400 | $225,600 | | Other Charges/Pass Thru | $0 | $0 | $0 | $946,200 | $0 | | Total | $3,753,500 | $3,775,300 | $3,825,000 | $4,521,000 | $4,170,700 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 58.0 | 55.1 | 57.0 | 57.5 | 56.0 | | Actual FTE | 54.3 | 55.2 | 56.0 | 50.1 | 0.0 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Managed Health Care Function The Bureau of Managed Health Care is responsible for implementing and operating the managed care initiative that includes contracts with managed care plans to serve the medical and mental health needs of Medicaid clients. The Bureau is also responsible for the development and implementation of a home and community-based waiver program and the Child Health Evaluation and Care program that is Utah's version of the federally-mandated Early Periodic Screening, Diagnosis and Treatment Program covering prevention, outreach, and expanded services for enrolled children. The Bureau also operates the Restriction Program for Medicaid clients that use multiple sources of care for the same service. This program requires clients to limit their use of services to certain providers rather than using multiple providers for the same service. Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $544,700 | $529,100 | $280,500 | $373,900 | $705,900 | | General Fund, One-time | $100,000 | $0 | ($8,100) | $0 | $0 | | Federal Funds | $2,063,900 | $2,308,800 | $2,072,700 | $1,561,200 | $1,586,500 | | American Recovery and Reinvestment Act | $0 | $111,300 | $158,900 | $0 | $0 | | Dedicated Credits Revenue | $143,300 | $183,100 | $0 | $0 | $0 | | GFR - Nursing Care Facilities Account | $0 | $0 | $0 | $547,200 | $0 | | Transfers - Within Agency | $565,000 | $561,500 | $914,000 | $650,000 | $914,000 | | Total | $3,416,900 | $3,693,800 | $3,418,000 | $3,132,300 | $3,206,400 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $2,716,400 | $2,941,100 | $2,859,500 | $2,535,300 | $2,603,800 | | In-state Travel | $15,100 | $12,400 | $9,700 | $7,900 | $10,100 | | Out-of-state Travel | $1,500 | $3,400 | $0 | $500 | $0 | | Current Expense | $630,500 | $673,300 | $508,600 | $560,300 | $550,000 | | DP Current Expense | $51,500 | $23,500 | $17,900 | $21,400 | $20,400 | | Other Charges/Pass Thru | $1,900 | $40,100 | $22,300 | $6,900 | $22,100 | | Total | $3,416,900 | $3,693,800 | $3,418,000 | $3,132,300 | $3,206,400 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 38.5 | 39.4 | 40.8 | 41.0 | 41.1 | | Actual FTE | 37.5 | 39.5 | 39.0 | 34.2 | 0.0 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Long-term Care Function The Bureau of Long-term Care serves as the administrative authority for the six Home and Community Based Waivers for the State. The Bureau directly administers the New Choices Waiver. The Bureau also oversees three Medicaid services: personal care, hospice services, and employment-related personal care services for individuals with disabilities working 40 hours or more per month. Additionally, the Bureau oversees the WorkAbility Program, which conducts outreach and education to support employment for people with disabilities. The Bureau is responsible for the prior authorizations required for some Medicaid services. The Bureau determines Clinical Eligibility (commonly known as Level of Care) and programmatic eligibility. These determinations are made by staff from the individual programs. The Department of Workforce Services determines overall Medicaid eligibility. Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $223,600 | $443,900 | $551,200 | $659,300 | $652,300 | | General Fund, One-time | $0 | $0 | ($3,500) | $0 | $0 | | Federal Funds | $1,327,900 | $1,544,900 | $1,717,100 | $2,095,900 | $1,622,400 | | Transfers - Within Agency | $300,000 | $46,900 | $200,000 | $200,000 | $200,000 | | Total | $1,851,500 | $2,035,700 | $2,464,800 | $2,955,200 | $2,474,700 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $1,162,700 | $1,197,400 | $1,905,500 | $2,187,000 | $1,972,600 | | In-state Travel | $19,200 | $9,900 | $4,000 | $2,100 | $4,000 | | Out-of-state Travel | $8,000 | $9,300 | $3,700 | $5,500 | $3,700 | | Current Expense | $439,600 | $510,200 | $362,900 | $395,900 | $305,600 | | DP Current Expense | $19,500 | $16,300 | $13,200 | $30,800 | $13,300 | | Other Charges/Pass Thru | $202,500 | $292,600 | $175,500 | $333,900 | $175,500 | | Total | $1,851,500 | $2,035,700 | $2,464,800 | $2,955,200 | $2,474,700 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 0.0 | 0.0 | 0.0 | 19.8 | 28.5 | | Actual FTE | 0.0 | 0.0 | 14.0 | 18.2 | 0.0 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Contracts Function This program deals with medical and dental consultants as well as Certified Public Accountant audits and reviews, which serve the Medicaid program. Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $357,500 | $830,400 | $647,700 | $669,800 | $794,700 | | Federal Funds | $42,430,100 | $38,872,600 | $34,455,100 | $7,088,400 | $1,361,500 | | Dedicated Credits Revenue | $3,838,700 | $2,399,800 | $0 | $6,209,800 | $8,700 | | Transfers - Intergovernmental | $0 | $124,000 | $0 | $0 | $0 | | Transfers - Medicaid - DHS | $0 | $9,472,500 | $8,405,000 | $200 | $32,800 | | Transfers - Medicaid - DWS | $0 | $24,583,900 | $24,347,400 | ($118,300) | $0 | | Transfers - Other Agencies | $7,664,700 | $0 | $0 | $0 | $0 | | Transfers - Within Agency | $26,879,900 | $240,600 | $52,500 | $4,200 | $42,500 | | Total | $81,170,900 | $76,523,800 | $67,907,700 | $13,854,100 | $2,240,200 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $0 | $9,000 | $80,000 | $0 | $0 | | Current Expense | $2,951,400 | $2,841,700 | $2,384,300 | $1,434,300 | $2,240,200 | | Other Charges/Pass Thru | $78,219,500 | $73,673,100 | $65,443,400 | $12,419,800 | $0 | | Total | $81,170,900 | $76,523,800 | $67,907,700 | $13,854,100 | $2,240,200 |
|---|
Subcommittee Table of ContentsProgram: Coverage and Reimbursement Function The Bureau of Coverage and Reimbursement Policy has the following four basic functions: - Research, analyze, formulate, and make recommendations for medical policy modifications and to develop new policy.
- Research, analyze, formulate, and make recommendations for pharmacy program policy modifications and to develop new policy.
- Formulate and process all State Plan changes and administrative rules.
- Determine appropriate reimbursement rates and methodology reflecting State and federal mandates as well as budget allocations.
Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $1,035,500 | $621,300 | $692,300 | $708,700 | $714,100 | | General Fund, One-time | $0 | $0 | ($5,600) | $0 | $0 | | Federal Funds | $4,104,500 | $2,229,400 | $1,317,700 | $1,100,000 | $1,233,600 | | Transfers | $0 | $333,300 | $0 | $0 | $0 | | Transfers - Within Agency | $852,600 | $0 | $356,500 | $54,600 | $100,000 | | Total | $5,992,600 | $3,184,000 | $2,360,900 | $1,863,300 | $2,047,700 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $3,622,400 | $1,972,400 | $1,710,700 | $1,626,600 | $1,894,700 | | In-state Travel | $3,500 | $1,100 | $200 | $0 | $300 | | Out-of-state Travel | $8,400 | $7,600 | $900 | $1,500 | $1,300 | | Current Expense | $2,242,800 | $1,151,000 | $607,100 | $196,600 | $109,300 | | DP Current Expense | $115,500 | $51,900 | $42,000 | $38,600 | $42,100 | | Total | $5,992,600 | $3,184,000 | $2,360,900 | $1,863,300 | $2,047,700 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 38.5 | 40.9 | 20.1 | 18.2 | 18.0 | | Actual FTE | 37.2 | 40.9 | 29.0 | 22.5 | 0.0 |
|
|
|
|
|
|
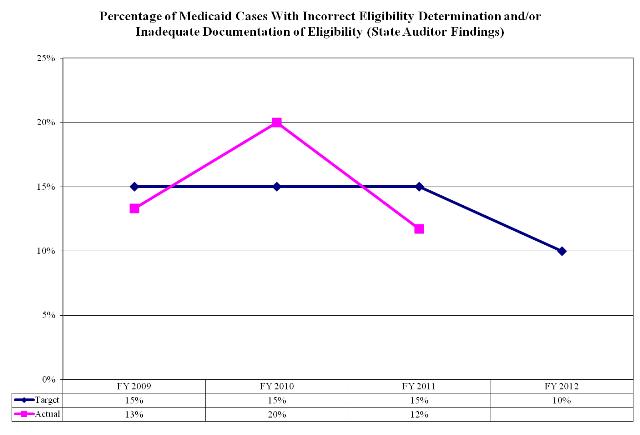
Subcommittee Table of ContentsProgram: Eligibility Policy Function The Bureau of Eligibility Policy is responsible to ensure Medicaid and Children's Health Insurance Program (CHIP) eligibility policy is in compliance with all State and federal statutes. It is also responsible to monitor the contract with the Department of Workforce Services to ensure Medicaid and CHIP eligibility determinations are done timely and accurately. The Department of Workforce Services determines the eligibility for nearly all clients to receive Medicaid services. The Department of Human Services contracts with the Department of Health to perform Medicaid eligibility. The Department of Human Services determines Medicaid eligibility for children in the custody of other states that reside in Utah, children in foster care, and for children receiving adoption assistance. Additionally, the Department of Human Services maintains Medicaid eligibility for children in the custody of Utah, but living in other states where they do not qualify for Medicaid. The Bureau operates the Buyout Program which determines if purchasing private health insurance would save the Medicaid program money for high risk clients. If so, Medicaid pays the health premiums for that plan. The Bureau houses the Medicaid Eligibility Quality Control Unit responsible for reviewing and verifying the accuracy of all Medicaid eligibility determinations. Additionally, the Bureau includes the State's Medical Review Board which determines an individual's disability status in order to qualify for Medicaid. Performance 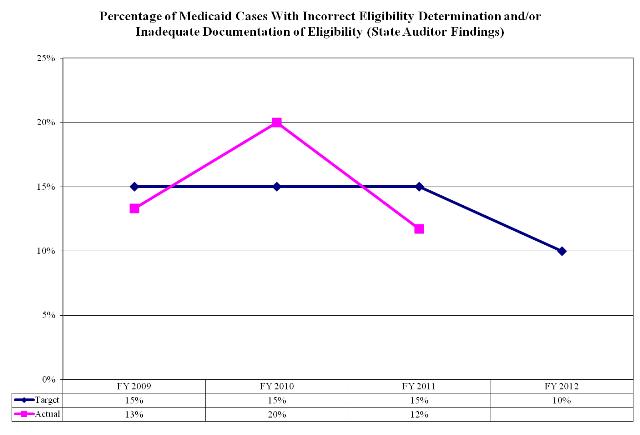 Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $723,900 | $494,400 | $305,200 | $131,600 | $105,100 | | General Fund, One-time | $107,000 | $0 | ($7,100) | $0 | $0 | | Federal Funds | $3,930,900 | $5,052,100 | $2,918,900 | $903,000 | $537,600 | | Dedicated Credits Revenue | $634,700 | $605,700 | $527,300 | $582,400 | $527,200 | | Transfers - Medicaid - DWS | $2,140,200 | $1,057,600 | $2,204,700 | $0 | $0 | | Transfers - Within Agency | $1,144,800 | $2,805,400 | $500,000 | $600,000 | $500,000 | | Total | $8,681,500 | $10,015,200 | $6,449,000 | $2,217,000 | $1,669,900 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $3,007,600 | $2,527,800 | $1,912,900 | $1,943,900 | $1,581,800 | | In-state Travel | $8,800 | $10,300 | $2,700 | $200 | $2,400 | | Out-of-state Travel | $6,400 | $1,200 | $0 | $0 | $0 | | Current Expense | $304,600 | $398,400 | $104,900 | $106,400 | $69,000 | | DP Current Expense | $84,200 | $47,800 | $19,100 | $19,300 | $16,700 | | Other Charges/Pass Thru | $5,269,900 | $7,029,700 | $4,409,400 | $147,200 | $0 | | Total | $8,681,500 | $10,015,200 | $6,449,000 | $2,217,000 | $1,669,900 |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 32.5 | 32.8 | 33.5 | 25.5 | 24.3 | | Actual FTE | 31.6 | 32.8 | 29.0 | 26.9 | 0.0 | | Vehicles | 2 | 2 | 0 | 0 | 0 |
|
|
|
|
|
|
Subcommittee Table of ContentsProgram: Department of Workforce Services' Seeded Services Function In FY 2008 funding and eligibility workers were transferred to the Department of Workforce Services as part of the Medicaid eligibility consolidation process. The funding in this program is the money that funds those efforts. Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Federal Funds | $0 | $0 | $0 | $20,678,100 | $23,582,300 | | Transfers - Medicaid - DWS | $0 | $0 | $0 | $20,678,100 | $23,582,300 | | Total | $0 | $0 | $0 | $41,356,200 | $47,164,600 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Other Charges/Pass Thru | $0 | $0 | $0 | $41,356,200 | $47,164,600 | | Total | $0 | $0 | $0 | $41,356,200 | $47,164,600 |
|---|
Subcommittee Table of ContentsProgram: Other Seeded Services Function Entities outside of the Department of Health contract with Medicaid, by sending some of their General Fund appropriations to the Division of Health Care Financing, which then uses those funds to draw down the matching federal Medicaid funds, then forwards all of the funds back to the original entities. This helps those entities leverage their funds by the federal match. A few examples of seeded services from State agencies include: The Department of Health assesses an administrative fee to all entities for coordinating their funds with the Medicaid program. The Department of Health explains how the amount of the assessment is calculated with the following three scenarios based on total funds matched:
3% of amounts less than $500,000
$15,000 and 2% of amounts above $500,000 up to $1,000,000
$25,000 and 1% of amounts above $1,000,000 A few examples of seeded services from non-State agencies include:
University of Utah to provide Graduate Medical Education training
Counties to provide mental health, substance abuse, as well as the Early Periodic Screening, Diagnosis and Treatment Program
School districts to provide skill development services
Funding Detail | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $0 | $0 | $0 | $15,800 | $0 | | Federal Funds | $0 | $0 | $0 | $11,579,200 | $11,368,300 | | Transfers - Medicaid - DHS | $0 | $0 | $0 | $8,788,900 | $10,635,900 | | Transfers - Medicaid - Internal DOH | $0 | $0 | $0 | $1,395,200 | $0 | | Transfers - Medicaid - USDB | $0 | $0 | $0 | $25,900 | $0 | | Transfers - Within Agency | $0 | $0 | $0 | $812,100 | $0 | | Total | $0 | $0 | $0 | $22,617,100 | $22,004,200 |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Other Charges/Pass Thru | $0 | $0 | $0 | $22,617,100 | $22,004,200 | | Total | $0 | $0 | $0 | $22,617,100 | $22,004,200 |
|---|
Subcommittee Table of ContentsProgram: Program Integrity Funding Detail Effective FY 2011, this program is now in the Executive Director's Office line item. | Sources of Finance | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | General Fund | $200 | $789,100 | $657,500 | $0 | ($1,900) | | General Fund, One-time | $0 | $0 | ($5,700) | $0 | $0 | | Federal Funds | $600 | $1,343,200 | $854,000 | $0 | ($3,400) | | Total | $800 | $2,132,300 | $1,505,800 | $0 | ($5,300) |
|---|
| | Categories of Expenditure | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Personnel Services | $800 | $2,090,700 | $1,442,100 | $0 | ($5,100) | | In-state Travel | $0 | $100 | $500 | $0 | $0 | | Out-of-state Travel | $0 | $400 | $0 | $0 | $0 | | Current Expense | $0 | $34,500 | $56,300 | $0 | ($200) | | DP Current Expense | $0 | $6,600 | $6,900 | $0 | $0 | | Total | $800 | $2,132,300 | $1,505,800 | $0 | ($5,300) |
|---|
| | Other Indicators | 2008
Actual | 2009
Actual | 2010
Actual | 2011
Actual | 2012
Approp | | Budgeted FTE | 0.0 | 0.0 | 26.5 | 0.0 | 0.0 | | Actual FTE | 0.0 | 0.0 | 13.0 | 0.0 | 0.0 |
|
|
|
|
|
|
Subcommittee Table of Contents |