Compendium of Budget Information for the 2011 General Session
| Social Services Appropriations Subcommittee | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Subcommittee Table of Contents | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Group: Social Services - Department of Health Line Item: Family Health and Preparedness Function The Division of Family Health and Preparedness assures and improves the quality of the Utah health care system, with an emphasis on care delivered to the most vulnerable populations. This function is fulfilled through the examination, analysis, and regulatory actions to improve service availability, accessibility, safety, continuity, quality, and cost. The Division directs the regulation and oversight of the health care industry. Division-wide improvement strategies include training, certification, licensing, and inspection. The Division also strives to assure that women, infants, children, and their families have access to comprehensive, coordinated, affordable, community-based quality health care. These health care services are available to all citizens of the State according to their ability to pay, but primary clients are women, infants, and children who have special health care needs and are low income. The Division coordinates efforts, identifies needs, prioritizes programs, and develops resources necessary to reduce illness, disability and death from adverse pregnancy outcomes and disabling conditions. The Division includes the Director's office and the following six bureaus: (1) Health Facility Licensing, Certification, and Resident Assessment, (2) Emergency Medical Services (EMS), (3) Child Care Licensing, (4) Preparedness Grants, (5) Children with Special Health Care Needs and (6) Primary Care. The Division also supports the Patient Safety Initiative, the Primary Care Grants Program, the Health Care Workforce Financial Assistance Program, and the Assistance to Persons with Bleeding Disorders Program. Additionally the Division provides pre-admission screenings for all Utah Medicaid recipients seeking nursing home or institutional care and promoting primary care services to underserved populations. Statutory Authority The Division of Family Health and Preparedness is governed by the Utah Health Code in Title 26 of the Utah Code.
Intent Language
Funding Detail For analysis of current budget requests and discussion of issues related to this budget click here.
Function The Office of the Director includes planning and budget analysis, coordination of intradivisional activities, oversight of the various bureaus, identification and implementation of information systems improvement, patient safety initiative, and Division liaison with other public and private agencies and organizations. The office consists of the Director, the Center for Multicultural Health, and the Financial Resources Program. The Center for Multicultural Health addresses health disparities among ethnic groups through health programs in the Health Department and in the community. The Center aims to foster accessible, high-quality programs and policies that help all racial and ethnic minorities in Utah achieve optimal health, dignity, and independence. The Center tries to increase public and health professional awareness of persistent racial/ethnic disparities and develop effective health policies and culturally competent programs that lead to better access to quality health care services and improved health status. The Financial Resources Program provides financial management for the Division by managing budgets, contracts and grants; ensuring compliance with financial policies and regulations; ensuring the accuracy of all financial transactions; and providing billing services for public services. Funding Detail Prior to FY 2011, the funding for this program was for two director's offices, one in the Health Systems Improvement line item and the other in the Community and Family Health Services line item.
Program: Maternal and Child Health Function The Bureau of Maternal and Child Health supports the Health Department's mission to reduce illness, disability and death among women of childbearing ages, children, and youth in the State. The Bureau identifies health concerns, prioritizes strategies to address needs, develops programs, coordinates efforts, and develops resources to address health issues for mothers and children. The Bureau of Maternal and Child Health provides leadership for many maternal and child health efforts in the State through its programs, contracts with local health departments and other entities, federal grant opportunities, and involvement at a national level to learn from other states about programs to apply in Utah. The Bureau is responsible for most maternal and child health issues, such as promotion of health among women of childbearing ages, health prior to pregnancy to promote healthy mothers and babies, access to health care before and during pregnancy, healthy weight and nutrition, oral health, and up-to-date immunization status. Additionally, the programs promote healthy children and adolescents through immunizations, oral health, healthy weight, and nutrition. The Bureau conducts surveillance and analysis of data related to pregnancy and factors associated with poor pregnancy outcomes, such as prematurity. The Bureau reviews maternal, fetal, and infant deaths. The information is used to identify factors that relate to prevention of poor outcomes and future deaths. The Bureau conducts surveillance and analysis of data related to children's health, such as dental screenings for young school-aged children to determine the degree of dental disease, or parents' experiences with health care for their children. The Bureau includes four programs that work to achieve the Bureau's goal of healthy mothers and children: Maternal and Infant Health, Data Resources, Oral Health, and the Women, Infants and Children Programs (WIC). The Bureau is responsible for the State Title V Maternal and Child Health Block Grant Application and Annual Report, Pregnancy Risk Assessment Monitoring System, and the USDA-funded WIC Program. The Bureau is also responsible for the State Early Childhood Comprehensive Systems Grant and the Head Start Collaboration Grant. Maternal and Infant Health (MIH) The mission of the Maternal and Infant Health Program (MIH) is to improve the health of women of childbearing age and their infants by reducing preventable illness, disability, and death related to pregnancy, birth, and infancy through the promotion of healthy lifestyles and optimal health care. The various components of the MIH include Prenatal/Family Planning, WeeCare, Pregnancy Risk Assessment Monitoring System (PRAMS), and the Perinatal Mortality Review (PMR) component. The program creates and disseminates pertinent health education messages that are identified through the program's various data collection resources. These messages are distributed via an Internet website (www.health.utah.gov/mihp), brochures, television, radio, poster displays and presentations at schools, churches, and health fairs. The program is guided by a strategic plan that includes nine outcome objectives:
The prenatal component of the Program seeks to improve access to prenatal care through expedited eligibility to Medicaid, enhanced prenatal and delivery services within Medicaid, and by covering prenatal care for uninsured women. The family planning component assures access to family planning services in underserved areas of the State, and also assures reproductive health services through technical assistance to and contracts with local health departments, community health centers, and other providers. The WeeCare component offers nurse case management of moderate and high-risk Public Employees Health Program pregnant participants throughout the State via telephone. The Pregnancy Risk Assessment Monitoring System (PRAMS) is a Centers for Disease Control and Prevention-developed, population-based surveillance system that queries a sample of Utah mothers about their experiences before, during and after pregnancy. Utah is among 39 states throughout the country who implement the survey. PRAMS is intended to help answer questions that birth certificate data alone cannot answer. Data are used to provide important information that can guide policy interventions, and other efforts to improve care and outcomes for pregnant women and infants in Utah. An example of how PRAMS data are being used is to educate prenatal care providers about the link between overweight/obesity and pregnancy outcomes. The Perinatal Mortality Review (PMR) component of the program is a process aimed at identifying and examining the factors that contribute to perinatal deaths (fetal, infant, and maternal) through the systematic evaluation of individual cases. Through individual case review, the PMR coordinator, in conjunction with a committee of perinatal professionals, identifies contributing factors that may have led to the death. Information is obtained through hospital records, public health records, autopsy reports, birth/death certificates and health care provider records. Committee members make recommendations based on findings that may lead to public health recommendations for changes that could improve the outcome of future cases. State Early Childhood Comprehensive Systems Grant and Head Start Collaboration Grant The program administers the State Early Childhood Comprehensive Systems grant, funded with federal Title V funds, to improve the system of services for children from birth to age eight by coordinating efforts of statewide agencies and organizations to ensure children are ready to enter school healthy and ready to learn. The Head Start-State Collaboration Office grant is designed to meet the increasingly complex and difficult challenges of improving long-term health outcomes for low-income children and their families and is funded with federal and State-match funds. The Data Resources Program (DRP) provides health data and information support to programs within Maternal and Child Health (MCH) and Children with Special Health Care Needs programs, local health departments, community-based health organizations, and the public. The program is two-pronged in its approach as it aims to (1) increase access to health information and data, and (2) provide analytic consultation, data training, and web services. DRP acts as a resource for MCH and CSHCN programs and provides expertise on research methodology, database design, survey development, and grant applications. The program also facilitates the coordination of multi-program projects and reports. The program also plays an active role in designing website and web-based applications for the Division of Family Health Preparedness and ensures that they are in compliance with Health Department and State web standards. DRP collaborates with programs to publish surveillance updates and research reports. An important responsibility of DRP is to provide coordination, compilation, and submission of the Federal Title V MCH Block Grant Application. Oral Health Program (OHP) The Oral Health Program (OHP) tries to improve the oral health status of Utah residents by developing, implementing, and promoting prevention and dental access programs at both the State and local health department levels. OHP dental caries prevention methods include community water fluoridation, fluoride mouth rinse programs, tooth sealant programs, and early childhood interventions. The evaluation and dissemination of statewide dental health surveys, Head Start data, and other Utah-specific dental health information by OHP provides needs assessment information for the State, local health departments, and dental societies in the State. The Program works with the Utah Dental Association and the Utah Dental Hygiene Association to promote the role of public health in promoting good oral health. In collaboration with the Utah Oral Health Coalition, the OHP has developed and maintains the Utah Oral Health Action Plan, which emphasizes implementation of appropriate prevention and access strategies for target populations and promotes development of policies for better oral health and improved oral health systems statewide. Additionally, the OHP encourages and facilitates the formation of local oral health coalitions by conducting needs assessments and oral health surveys, providing technical consultation, and reporting progress toward Healthy People 2010 oral health objectives. The OHP collaborates with local health departments and community health centers and partners with many community public health and private practice dental and health professionals, stakeholders, and advocates to implement programs which serve the needs of local communities. The OHP has developed and maintains an oral health website that provides educational and resource information for public and private partners as well as the general population of the State. Women, Infants and Children (WIC) Women, Infants and Children (WIC) is a federally-funded program designed to provide supplemental food and nutritional education to pregnant, breast-feeding or postpartum women, infants and children up to five years of age. Applicants must meet the following criteria to be certified and eligible for WIC authorized foods:
Funding Detail Effective FY 2011 the immunization program is now part of the Epidemiology Program within the Disease Control and Prevention line item. Immunization was previously part of the Maternal and Child Health Program.
Program: Public Health Preparedness Function The federal government funds a nationwide grant program for bioterrorism preparedness through the Centers for Disease Control and Prevention (CDC). The grant is broken down into six categories under nine preparedness goals. They are: Prevent:
In addition to the CDC Bioterrorism grant, the Health Resources and Services Administration Hospital Preparedness Bioterrorism Grant provides money to Utah. This grant is designated for hospitals to increase training, education, and supplies. The grant is broken into the following priority areas:
Funding Detail
Program: Children with Special Health Care Needs Function The Bureau of Children with Special Health Care Needs (CSHCN) encompasses ten programs serving special needs children: Baby Watch Early Intervention Program, Fostering Healthy Children, Developmental Consultative Services, Utah Birth Defect Network, Newborn Screening Program, Specialty Services Program, Neonatal Follow-up Program, Pregnancy RiskLine, Child Health Advanced Records Management, and Technology Dependent Waiver/Family Involvement. CSHCN programs work to reduce preventable death, disability, and illness due to chronic and disabling conditions by providing access to affordable high-quality health screening, specialty health care, and coordination of health services. Bureau programs try to improve the system of care for Utah children with special needs through direct or population-based services and the promotion of system infrastructure building. Baby Watch Early Intervention Program
Developmental Consultative Services
Utah Birth Defect Network (UBDN) The Utah Birth Defect Network (UBDN) is a statewide surveillance system monitoring the occurrence of major structural birth defects in Utah. The UBDN uses this information to assess the prevalence of birth defects occurring in Utah; conduct epidemiological studies to determine risk factors; educate women and health care providers about these risk factors; evaluate whether education has decreased specific birth defects; and respond to reported clusters of birth defects. Birth defects are the leading cause of infant mortality, contribute to premature births, and are the major reason for hospitalizations during the first year of life. There are economic costs to families and society for children born with birth defects and the costs extend beyond medical and surgical care to behavioral and educational service issues. Because the cause of most birth defects are unknown, UBDN participates in a national study of birth defects to increase understanding of modifiable risk factors. The UBDN's efforts are directed toward primary prevention of birth defects by monitoring occurrence, conducting educational outreach, and participating in collaborative epidemiologic studies. Evaluation of the UBDN epidemiologic data provides information in order to assess risk factors for birth defects and develop primary prevention activities directed at reducing these risk factors. Primary prevention activities target high-risk populations. The effectiveness of the prevention programs are evaluated through the continuous tracking of all major birth defects statewide. The UBDN serves as a resource and referral system for families and physicians. UBDN measures: (1) accurate and timely tracking of birth defects statewide; (2) folic acid educational campaign and evaluation of neural tube prevalence over time to evaluate effectiveness of prevention activities; and (3) estimated number of individuals reached through general education and outreach activities.
The Pregnancy RiskLine (PRL) provides information regarding exposure to drugs, chemicals, and infections in pregnancy and lactation and the possible effect on the developing fetus, breast-fed, infant and mother. The Pregnancy RiskLine was established to provide health care practitioners and consumers with accurate, up-to-date information regarding potential risks to a fetus or breast-fed infant in order to prevent unjustified anxiety leading to unnecessary abortions, costly prenatal and postnatal screening, diagnostics, and testing of an exposed fetus or infant. Major goals of the program are aimed at prevention of poor pregnancy outcomes and adverse health effects in children. The desired outcomes are intended to prevent low birth weight, infant mortality, and birth defects. By offering accurate and current information about fetal effects of maternal exposure to medications, drugs, chemicals, infections and diseases, the PRL may prevent untoward effects of some of these agents on a developing fetus, resulting in a decreased incidence of low birth weight, infant mortality, and birth defects. Child Health Advanced Records Management (CHARM) Currently, data exists in an array of public and private health sectors and each database serves its own users, but with no capacity to share data across organizations or health programs. Services are often not coordinated and typically do not provide a network of care for families resulting in many children not receiving critical follow-up. The Child Health Advanced Records Management (CHARM) Project is a coordinated, Department-wide effort to create an electronic virtual health profile for every child in Utah that allows real-time digital access and data sharing among appropriate health care programs and partners. The CHARM vision is to create a shareable repository of child-specific public health information with secure role-based confidential access to a comprehensive set of integrated public health data accessible by people with a need to know, that promotes timely and efficient access to needed services, and supports program planning and evaluation. Integrating the State's health care databases provides for immediate access to information that is stored in specific databases to track and monitor health status for children and their families. In the last few years, CHARM has linked the databases from Vital Records, (Birth and Death Certificates), Utah Statewide Immunization Information System, Early Hearing Detection and Intervention, Baby Watch Early Intervention Program ,and the Office of Recovery Services. The Newborn Screening (heelstick) Program will be integrated next. Following the integration of this program, the UBDN and clinical information from the Neonatal Follow-up Program will also be linked to CHARM. Through data-sharing and tracking among integrated programs, CHARM's goal is to reduce the number of children lost to follow up statewide and provide more accurate and timely information to the child's medical home through web access. The Department is developing strategic and technical implementation plans to incorporate the CHARM data integration system into the Utah statewide Department's Clinical Health Information Exchange (cHIE) initiative. Funding for this project has come from braiding multiple funding streams including Health Resources Services Administration grants, Centers for Disease Control and Prevention grants, and the Maternal and Child Health Block Grant. Management of the funds is performed by an oversight committee (CHARM Governing Board) to ensure accountability and coordinated use. The CHARM Project is managed by a 'hands on' work group consisting of a program manager, an operations manager, and technical data services and support. Technology Dependent Waiver/Family Involvement The Division of Health Care Finance shares the responsibility for the day-to-day administrative activities for Utah's Waiver for Technology Dependent, Medically Fragile Individuals with the Technology Dependent Waiver Program. The waiver program tries to prevent institutionalization and to facilitate transition from an institutional setting to a home and community-based setting for technology dependent, medically-fragile children with complex medical conditions. The Family Involvement Program/Family Voices provides information, training, and support regarding health care and community services to families of children and youth with special health care needs. Family Voices facilitates partnerships between families and professionals on behalf of children and youth with special health care needs. Performance 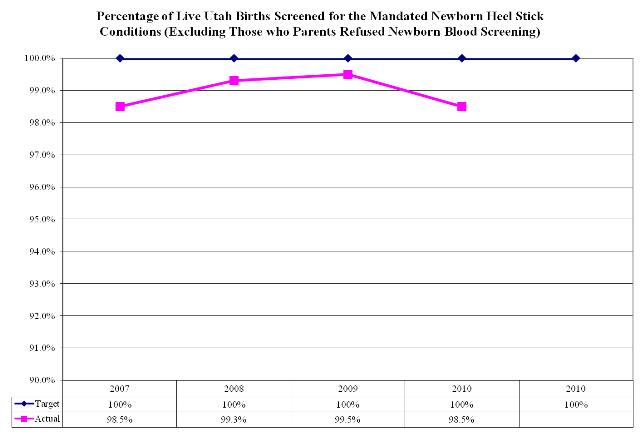 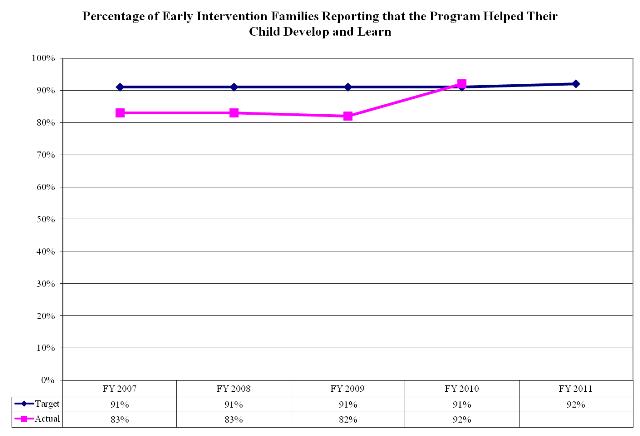 Funding Detail
Program: Emergency Medical Services Function The Bureau of Emergency Medical Services is a leadership team functioning as a resource and providing assurance of a quality emergency medical system in the State. The Bureau of Emergency Medical Services (EMS) has as its mission to promote a statewide system of emergency and trauma care to reduce morbidity and mortality, through prevention, awareness, and quality intervention. The Bureau implements this mission by:
EMS Grants Program The portion of the criminal fines and forfeitures surcharge that is allocated to EMS has restrictions on its usage established in UCA 26-8a-207. After funding staff support, administrative expenses, and trauma system development, the Bureau then allocates at least 25% (actual percentage determined by the Emergency Medical Services Committee) for per capita block grants for emergency medical services at the county level, determined by population and number of EMS employees, and the remaining percentage as competitive grants distributed to applicants based on the guidelines approved by the Emergency Medical Services Committee. EMS Certification EMS personnel must be certified to meet a statewide standard for emergency medical services. These statewide standards for training levels are based upon the standards and curricula established by the National Highway Traffic Safety Administration. The differences between levels of certification relate to the types and extent of procedures that may be performed by the EMS personnel, such as starting IV fluids, administering medications, or placing tubes to open a patient's airway. Performance 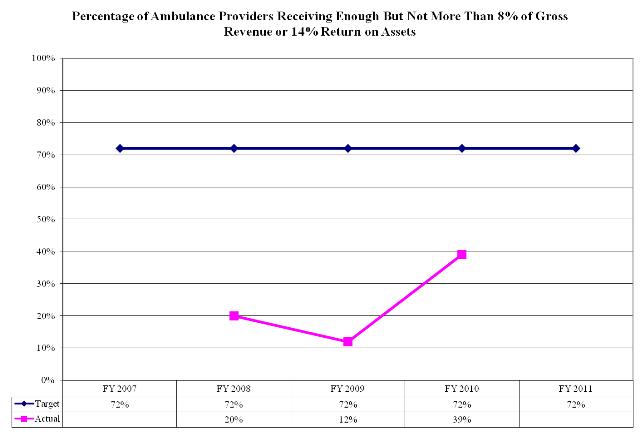 Funding Detail
Program: Facility Licensure, Certification, and Resident Assessment Function The Bureau of Health Facility Licensing, Certification, and Resident Assessment has the responsibility for licensing and inspecting health care facilities including hospitals, nursing homes, Intermediate Care Facilities for the Mentally Retarded, home health agencies, assisted living facilities and many other provider types. Additionally, the Bureau inspects those health care facilities choosing to be certified for Medicare/Medicaid programs. The Bureau also investigates complaints made about these providers, and performs pre-admission/continued stay health screenings for all Utah Medicaid recipients seeking nursing home or institutional care. The Bureau performs background screening for all direct care staff of all nursing homes, small health care facilities, assisted living, home health agencies, hospice agencies, and end stage renal disease facilities. The Bureau is responsible for managing two federal grants: Title 18 (Medicare) Certification Grant and Title 19 (Medicaid) Certification. These grants are funded at different federal matching rates. Title 18 Certification is 100 percent federally-funded and Title 19 is matched at either 75 percent or 50 percent Federal Financial Participation. In addition, the Bureau participates in the regular Title 19, general Medicaid administration program. This program is matched at 75 percent or 50 percent Federal Financial Participation. Overall, the average match rate is 87.5 percent federal and 12.5 percent State. The Bureau reviews building plans for new construction and remodeling of health care facilities. Some of the building design and construction requirements for health care facilities that are much more stringent than private structures include: ventilation systems, sprinkler systems, size of hallways, access and egress points, adequacy of plumbing, emergency power supplies, and many others. Intent Language
Performance 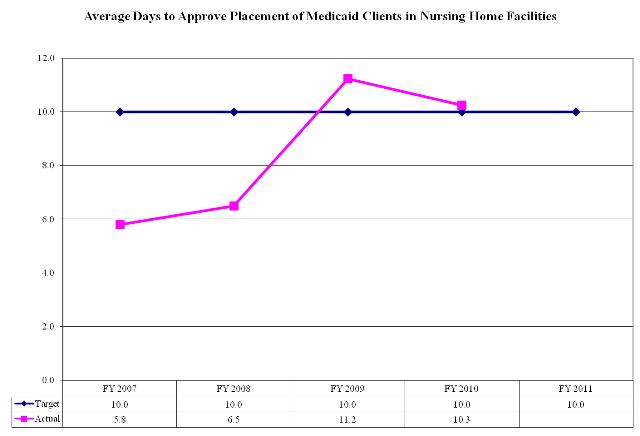 Funding Detail
Function The Bureau of Child Care Licensing is responsible for protecting the health and safety of children in regulated child care programs by: establishing and enforcing health and safety rules for child care programs, assisting providers in meeting the health and safety rules, and providing the public with accurate information about regulated child care. The Bureau of Child Care Licensing implements this mission by inspecting child care facilities to ensure compliance with licensing rules, investigating complaints about regulated providers, and providing training on the licensing rules. Child care licensing rules include requirements for the physical facility, personnel, emergency preparedness, supervision of children, child health and nutrition, injury prevention, and infection control. A provider/facility may be issued a citation if the facility is found to be in violation of licensing rules. If cited findings are not corrected, then a civil money penalty is assessed. These funds are used to fund State training for child care providers. The categories of providers regulated by the Bureau include Child Care Centers, Hourly Child Care Centers, Licensed Family Child Care (in-home), and Residential Certificate Care (in-home). In general anyone caring for five or more unrelated children must comply with licensing requirements. UCA 26-39 directs that the child care facilities under the supervision of the following groups are exempt from licensing requirements:
Intent Language
Funding Detail
Function The Bureau of Primary Care includes several programs focusing on health care for some of Utah's most vulnerable populations. Office of Primary Care and Rural Health The Office of Primary Care and Rural Health serves as a resource for Utah's rural, multi-cultural, and medically underserved communities. The office works with communities that need assistance in conducting needs assessments, recruiting health care professionals, grant writing, identifying sources of funding, and implementing other projects related to decreasing health disparities and increasing access to primary health care. The office also serves as the federally-funded State Office of Rural Health and as the Primary Care Office for the federal National Health Service Corps and the Conrad State 30 J-1 Visa Waiver Program. The office tries to recruit and retain health care professionals to work in medically underserved areas of Utah. The Rural Hospital Flexibility Grant Program assists in strengthening rural health by: (1) helping small hospitals be licensed as critical access hospitals, which qualifies them for cost-based reimbursement for Medicare acute inpatient and outpatient services, (2) encouraging the development of rural-centric health networks, and (3) offering grants to help implement a critical access hospital program in the context of broader initiatives to strengthen the rural health care infrastructure. The Small Rural Hospital Improvement Grant Program assists small rural hospitals to help them: (1) pay for costs related to the implementation of Medicare Prospective Payment Systems, (2) comply with provisions of Health Insurance Portability and Accountability Act (HIPAA), (3) reduce medical errors, and (4) support quality improvement. Primary Care Grants Program The State Primary Care Grants Program for Medically Underserved Populations makes grants to public and non-profit entities for the cost of providing primary health care services to medically underserved populations. The program strives to decrease the number of individuals without access to appropriate, high quality, effective primary health care by making these grants to qualified provider organizations. The program targets Utah's low-income populations, who have no health insurance, or whose health insurance does not cover primary health care services and do not qualify for Medicare, Medicaid, CHIP, or other government insurance programs. The scope of this program includes populations in medically underserved areas, individuals with chronic diseases, the homeless, Native Americans, seasonal and migrant farm workers, and other disadvantaged groups. Assistance to Persons with Bleeding Disorders The Assistance to Persons with Bleeding Disorders Program makes grants available to assist persons with bleeding disorders with the cost of obtaining services for hemophilia or the cost of insurance premiums for coverage of hemophilia services. The program assists persons who meet the following criteria:
The Patient Safety Initiative coordinated with the Utah Hospital Association and HealthInsight, provides monitoring of numerous health outcomes in an effort to improve the safety of Utah's health care delivery systems. Office of American Indian/Alaska Native Health Affairs The Office of American Indian/Alaska Native Health Affairs in cooperation with Utah Medicaid supports efforts to improve the health status of this population and address consultation requirements for these government-to-government relationships. Intent Language
Funding Detail
|