The Bureau of Eligibility Policy is responsible to ensure Medicaid and Children's Health Insurance Program (CHIP) eligibility policy is in compliance with all State and federal statutes. It is also responsible to monitor the contract with the Department of Workforce Services to ensure timely and accurate Medicaid and CHIP eligibility determinations. The Department of Workforce Services determines the eligibility for nearly all clients to receive Medicaid services. The Department of Human Services contracts with the Department of Health to perform Medicaid eligibility. The Department of Human Services determines Medicaid eligibility for children in the custody of other states that reside in Utah, children in foster care, and for children receiving adoption assistance. Additionally, the Department of Human Services maintains Medicaid eligibility for children in the custody of Utah, but living in other states where they do not qualify for Medicaid.
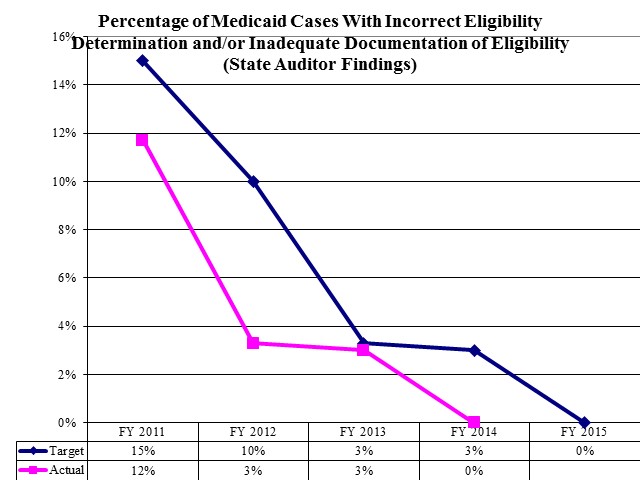
Percentage of Medicaid cases with incorrect eligibility determination and/or inadequate documentation of eligibility (State Auditor findings)
The Bureau operates the Buyout Program which determines if purchasing private health insurance would save the Medicaid program money for high risk clients. If so, Medicaid pays the health premiums for that plan. The Bureau houses the Medicaid Eligibility Quality Control Unit responsible for reviewing and verifying the accuracy of all Medicaid eligibility determinations. Additionally, the Bureau includes the State's Medical Review Board which determines an individual's disability status in order to qualify for Medicaid.
The Department has a website that allows registered providers to verify a client's Medicaid eligibility and plan enrollment electronically. The website will also indicate if a client has co-pays to receive services.
COBI contains unaudited data as presented to the Legislature by state agencies at the time of publication. For audited financial data see the State of Utah's Comprehensive Annual Financial Reports.