The Children's Health Insurance Program (CHIP) provides health insurance coverage to uninsured children up to age 19 living in families whose income is between 139 and 200 percent of the Federal Poverty Level (FPL). Additionally, eligible children must: (1) not have access to affordable health insurance, (2) not have voluntarily terminated private health insurance within the last 90 days, and (3) be U.S. citizens or legal residents. There is no asset test for CHIP eligibility. For more information please visit http://health.utah.gov/chip/howtoapply.htm.
During the 2015 General Session, the Legislature appropriated for Fiscal Year 2016, $79,360,700 from all sources for Children's Health Insurance Program. This is a 4.3 percent reduction from Fiscal Year 2015 revised estimated amounts from all sources. The total includes $1,579,200 from the General/Education Funds, a reduction of 76.4 percent from revised Fiscal Year 2015 estimates.
In addition to statewide compensation and internal service fund cost increases, the following appropriation adjustments were made during the 2015 General Session:
CHIP Performance Measures
As of June 2014 CHIP had 15,600 clients in one of two health plans. Select Health had 60% of clients and Molina had 40% of clients on a full-risk contract. Below are some performance measures from client surveys of FY 2013 CHIP providers as compared to national averages. The full reports can be found at http://health.utah.gov/myhealthcare/report/cahps/2013/. The three charts where clients rated their service are explained by the report with: "The…survey asked members to rate different characteristics of their health plan on a scale of 0 ("worst plan possible") to 10 ("best plan possible"). The charts below show the percentage of members who gave their plan a score of 8, 9, or 10."
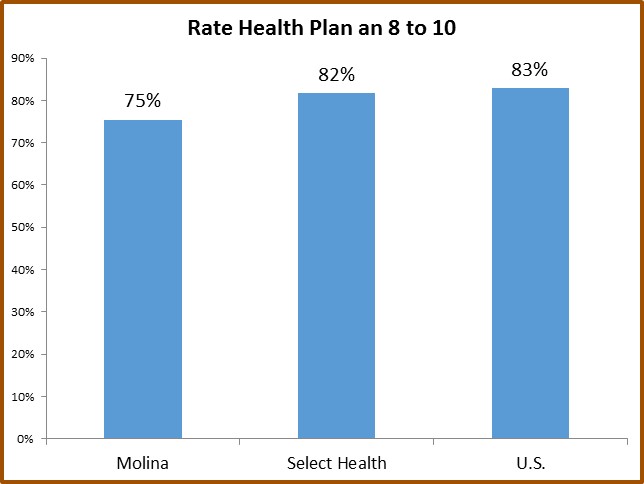
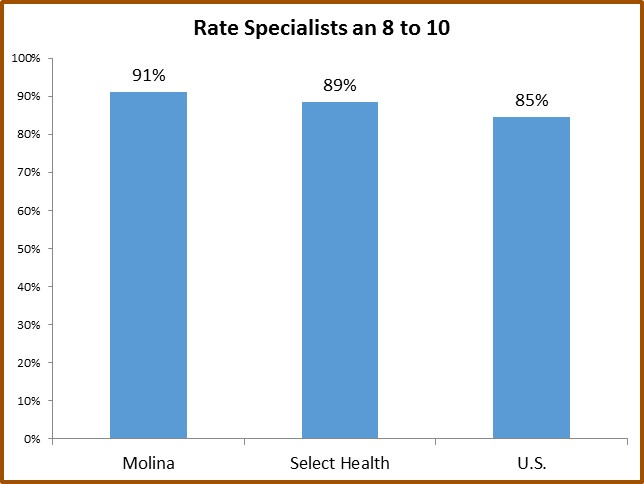
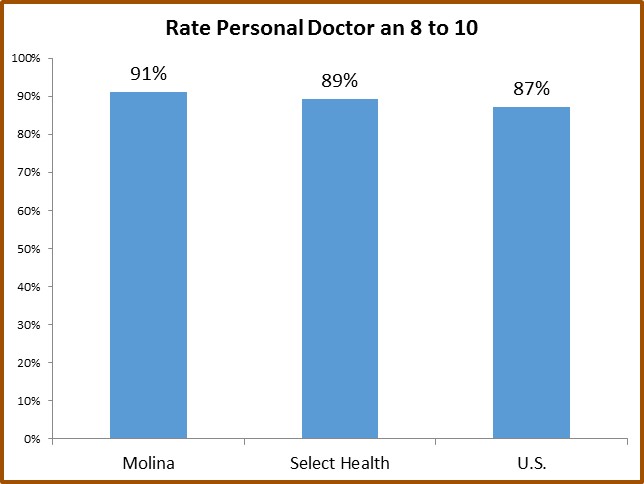
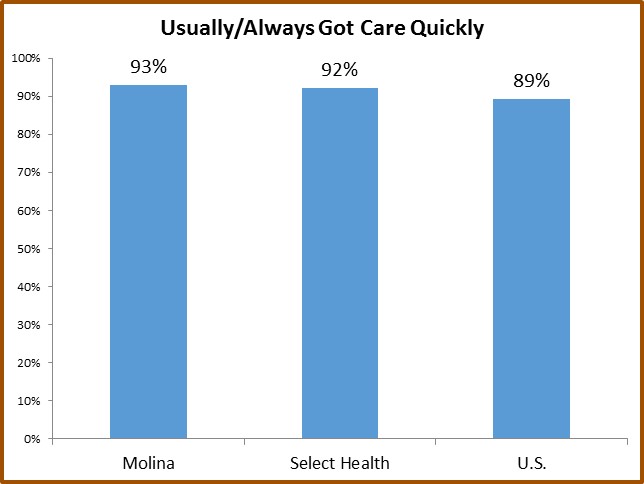
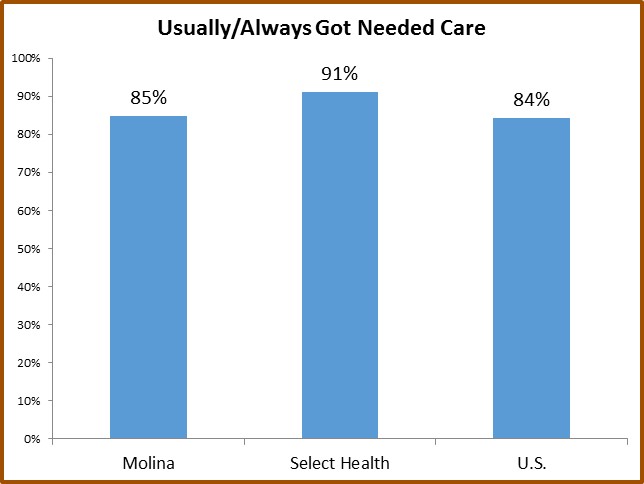
Both Select Health and Molina ranked higher than the U.S. average for four of the five measures. Molina ranked higher than Select Health in three of the five measures.
CHIP FY 2014 Expenditure and Enrollment Overview
In FY 2014, the average monthly cost per CHIP child was $150. The average monthly cost for CHIP kids now enrolled in Medicaid was $183 (changes mandated by the federal Affordable Care Act). Approximately 72 percent of CHIP children live in Davis, Salt Lake, Weber, and Utah counties. Approximately 57 percent of children eligible for CHIP became eligible for Medicaid in 2014.
Caseloads in Utah's Premium Partnership for Health Insurance
Caseloads for Utah's Premium Partnership for Health Insurance went from 275 children in FY 2013 to 282 children in FY 2014, an increase of 3%. The program has ongoing efforts to encourage people to apply for the program. This program pays monthly up to $120 per child to pay the premiums of qualifying employee-sponsored health insurance. Additionally, another $20 per month per child can be obtained for employee-sponsored dental coverage. About 80% of participating children receive both subsidies. Children who qualify can live in families that make up to 200% of the Federal Poverty Level (a little under $4,000 monthly for a family of 4 in 2014).
In FY 2014 CHIP spent $0.09 of every $1 on administration for the costs of the Departments of Health and Workforce Services. Premiums, shown as dedicated credit revenue, covered about 2% of the program's costs.
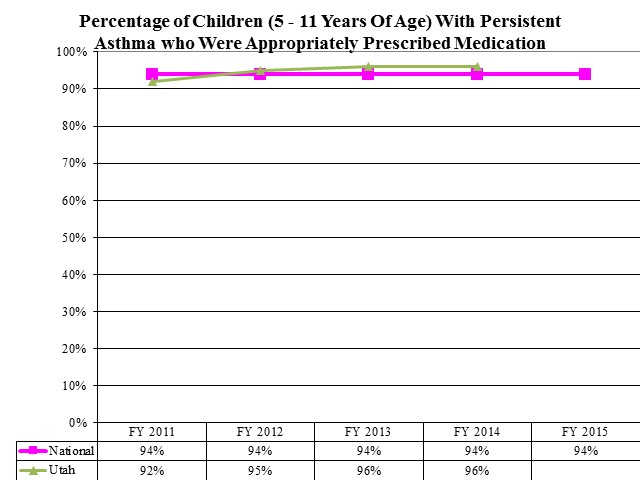
Percentage of Children (5 - 11 Years Of Age) With Persistent Asthma who Were Appropriately Prescribed Medication
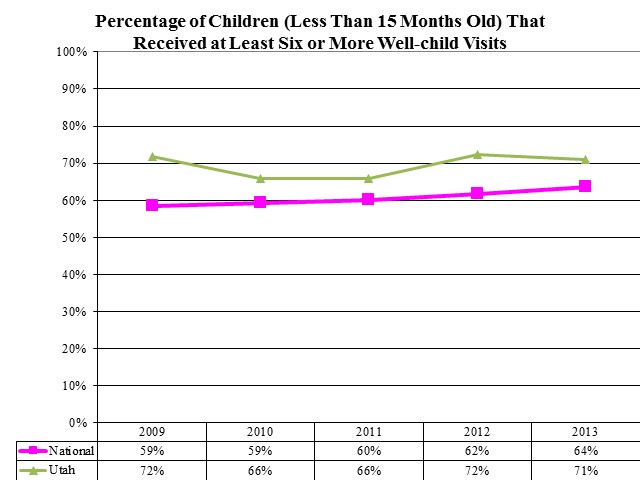
Percentage of Children (Less Than 15 Months Old) That Received at Least Six or More Well-child Visits
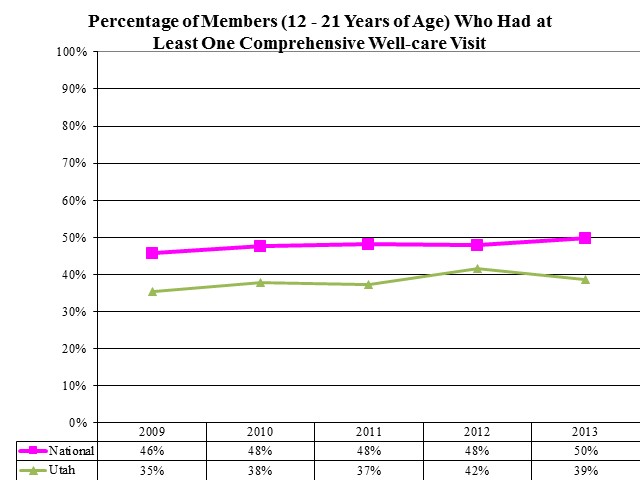
Percentage of Members (12 - 21 Years of Age) Who Had at Least One Comprehensive Well-care Visit
Utah's Premium Partnership for Health Insurance (UPP) allows families to receive a partial reimbursement of their health insurance premium using CHIP funds if enrolled in their employer's health care coverage or in COBRA continuation coverage. This line item has the funding for children on UPP. UPP pays monthly up to $120 per child to pay the premiums of qualifying employee-sponsored health insurance and up to $20 monthly for qualifying employee-sponsored dental insurance. Children that do not have access to affordable employee-sponsored dental insurance may enroll in CHIP dental coverage. Children who qualify can live in families that make up to 200% of the Federal Poverty Level. The Medical Optional Services line item has the funding for adults on UPP.
The major portion of the funding for CHIP comes from federal funds. The authorized level of federal funds is tied to the State's Medicaid rate, but at an enriched level. Because the State of Utah has a relatively high Medicaid rate, the CHIP services match rate is also fairly high as compared to the national average. CHIP clients receive services from one of two managed care plans operating under fully risk-based, capitated contracts.
The benefit package for CHIP emphasizes prevention and is based on the benefit package offered by the health maintenance organization in the State with the largest commercial enrollment. There is no cost to clients for well-child exams and immunizations. Some services require cost sharing, which varies depending on a family's income level. Cost sharing by clients is actuarially equivalent to the cost sharing in private health plans for families with incomes from 151 to 200 percent FPL, but may not exceed 5 percent of the household's gross income in any given year. CHIP provides two cost sharing plans based on income: Plan B between 139% and 150% of FPL and Plan C between 151% and 200% of FPL. The federal government places additional limits on cost sharing for the families on Plans B.
For analysis of current budget requests and discussion of issues related to this budget click here.
The monthly caseload is the number of children served by the Children's Health Insurance Program.
COBI contains unaudited data as presented to the Legislature by state agencies at the time of publication. For audited financial data see the State of Utah's Comprehensive Annual Financial Reports.