The federal Centers for Medicare and Medicaid Services (CMS) designates which services in Medicaid are optional. An optional service means that a state does not have to provide the service for most Medicaid clients. These 38 optional services are eligible for the State's federal matching funds. These services include pharmacy, dental, ambulatory surgery, chiropractic, podiatry, physical therapy, vision care, substance abuse treatment, hearing, speech, dialysis clinics, surgical centers, alcohol and drug clinics, intermediate care facilities individuals with intellectual disabilities, personal care, hospice, and private duty nursing. As noted in the Medicaid Mandatory Services section, some of these services may be mandatory for certain populations or in certain settings. While the service as a whole may be optional, once the State elects to offer that service to a specific group, it must make it available to all qualified eligibles in that group. Alternatively, when the State decides to stop or start providing a particular service, it must submit a State Plan Amendment to the Centers for Medicare and Medicaid Services, notify clients thirty days in advance, and provide a public notice at least one day before the change.
During the 2015 General Session, the Legislature appropriated for Fiscal Year 2016, $960,202,000 from all sources for Medicaid Optional Services. This is a 1.8 percent increase from Fiscal Year 2015 revised estimated amounts from all sources. The total includes $123,644,400 from the General/Education Funds, an increase of 16.8 percent from revised Fiscal Year 2015 estimates.
In addition to statewide compensation and internal service fund cost increases, the following appropriation adjustments were made during the 2015 General Session:
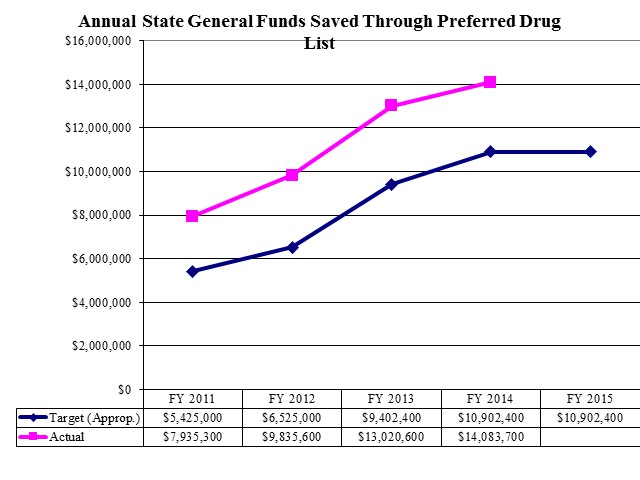
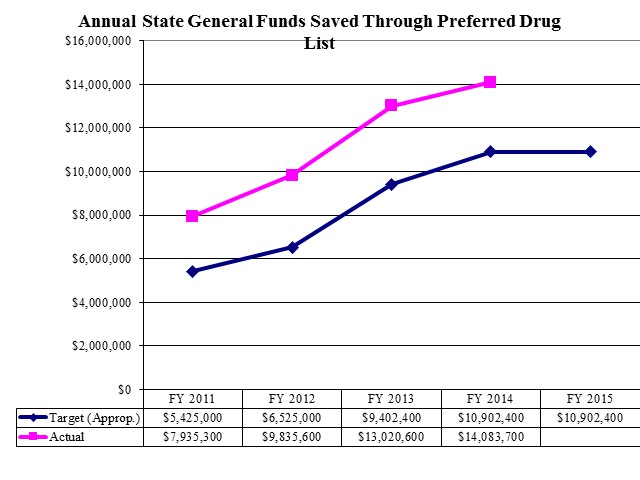
Cumulative State General Funds Saved Through Preferred Drug List
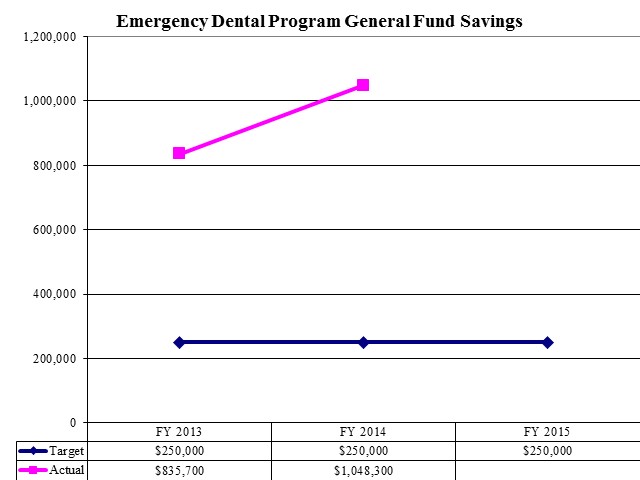
Emergency Dental Program General Fund Savings
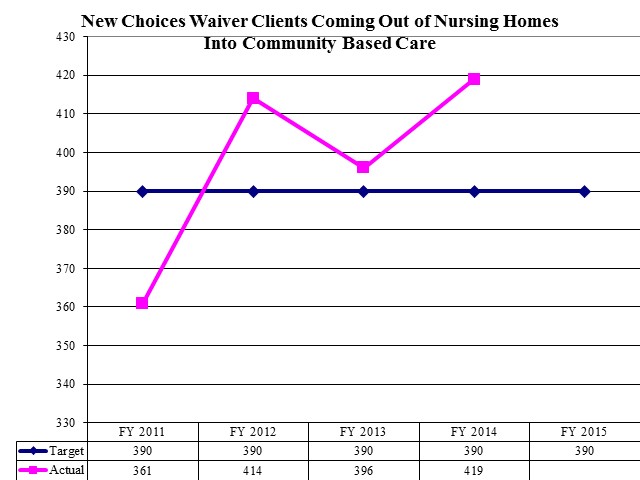
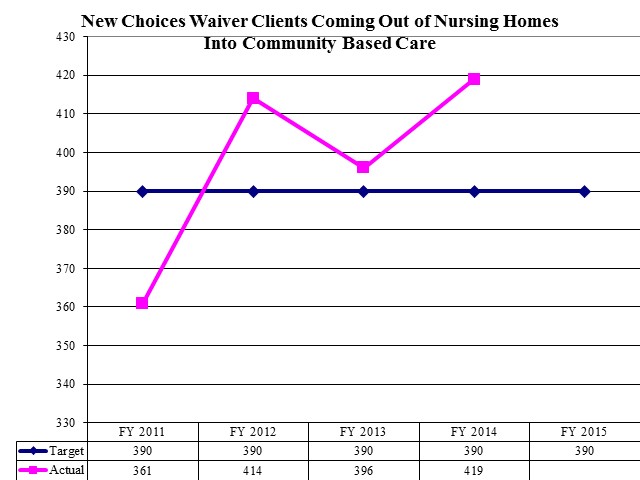
New Choices Waiver Clients Coming Out of Nursing Homes Into Community Based Care
There are 11 optional services that Utah does not provide in its Medicaid program: adult dental services, home health occupational therapy; home health speech and language; eyeglasses; home health audiology; speech, hearing and language; nurse anesthetist; chiropractor; Program of All-Inclusive Care for the Elderly; respiratory care; and qualified Religious Nonmedical Health Care Institutions.
There are 12 programs within the Medicaid Optional Services line item: Capitated Mental Health Services, Pharmacy, Non-service Expenses, Home and Community Based Waivers Services, Dental Services, Intermediate Care Facilities for Individuals with Intellectual Disabilities, Buy-in/Buy-out, Hospice Care Services, Vision Care, Disproportionate Share Hospital Payments, Clawback Payments, and Other Optional Services. Medicaid Optional Services also includes the Primary Care Network and Utah's Premium Partnership for Health Insurance.
The Division of Aging and Adult Services has a Medicaid waiver to pay for some services in home and community-based settings. The waiver diverts some elderly people from nursing facility care. The waiver has an enrollment cap and maintains a waiting list for those seeking to receive services. Based on a needs assessment, an individual may receive some or all of the following services: adult companion, adult day health, case management, chores, emergency response systems, environmental accessibility adaptations, fiscal management, home delivered supplemental meals, homemaker, medication reminder systems, non-medical transportation, personal attendant program training, personal attendant, respite care, specialized medical equipment, and supportive maintenance home health aide.
Historically, the Legislature has directed the Department of Human Services to maximize federal funds, often through accessing Medicaid for Human Services when possible. Certain services and clients of the Department of Human Services qualify for funding under the Medicaid Program. Some of the programs that receive Medicaid funding are: the Utah State Hospital, the Utah State Developmental Center, Home and Community Based Waivers in the Divisions of Aging and Adult Services, Services for People with Disabilities, Juvenile Justice Services, and Child and Family Services.
Medicaid Work Incentive Program
Utah has opted to cover individuals with disabilities who are working through the Medicaid program. The program is called the Medicaid Work Incentive Program. To qualify an individual with disabilities who is working can have countable income up to 250% of the Federal Poverty Level. Countable income generally is half of all earned income. Based on the individuals' income, they pay the following percentage of their countable income in exchange for Medicaid services:
- 5% for incomes from 100% to 110% of the Federal Poverty Level.
- 10% for incomes from 110% to 120% of the Federal Poverty Level.
- 15% for incomes from 120% to 250% of the Federal Poverty Level.
For analysis of current budget requests and discussion of issues related to this budget click here.
COBI contains unaudited data as presented to the Legislature by state agencies at the time of publication. For audited financial data see the State of Utah's Comprehensive Annual Financial Reports.