The Division of Medicaid and Health Financing is the administrative agency for Utah's Medical Assistance Programs (Medicaid, Children's Health Insurance Program, Utah's Premium Partnership for Health Insurance, and Primary Care Network). As per federal requirements, all funding for Medicaid must flow through the Department of Health via a memorandum of understanding for all functions performed by other entities whether State, non-profit, for profit, local government, etc. About 32% of clients receive their medical services from any willing provider who bills Medicaid directly. The other 68% of clients receive most of their medical services through four contracted health plans who handle the billing and case management services of their clients.
During the 2015 General Session, the Legislature appropriated for Fiscal Year 2016, $108,839,600 from all sources for Medicaid and Health Financing. This is an 8 percent reduction from Fiscal Year 2015 revised estimated amounts from all sources. The total includes $5,064,300 from the General/Education Funds, a reduction of 13.9 percent from revised Fiscal Year 2015 estimates.
In addition to statewide compensation and internal service fund cost increases, the following appropriation adjustments were made during the 2015 General Session:
Issue Brief - 2014 General Session - Medicaid Spending Statewide
Medicaid's Inspector General (OIG) - UCA 63A-13-502 directs that: "The inspector general of Medicaid services shall provide the report described in Subsection (1) to the Executive Appropriations Committee of the Legislature and to the governor on or before October 1 of each year. The inspector general of Medicaid services shall present the report described in Subsection (1) to the Executive Appropriations Committee of the Legislature before November 30 of each year." The report is available at http://le.utah.gov/interim/2014/pdf/00004431.pdf. Below are some quotes from the report:
- "Taxpayer Funds Collected $11,570,604"
- "Utah OIG completed 31 provider outreach trainings, visiting nearly all Utah counties, and 4 professional groups during FY 2014, to help educate providers and reduce future instances of waste, abuse, and fraud."
- "The Special Investigations Unit conducted 1,287 investigations, incorporating 8,418 medical claims in FY 2014. Investigations included Durable Medical Equipment, Pharmacy, Home Health, Hospitals, Hospice, Physicians and Dental providers. The 8,418 medical claims included: 3,004 that required no action, 3,202 that received notification of a Utah OIG action, and 2,216 are currently in various stages of the review process."
- "The Performance Audit team released 15 audits with 56 recommendations to Medicaid in FY 2014. Medicaid agreed with all 56 recommendations and has already implemented 22 of them; the other 34 have scheduled implementation dates. The Utah OIG Audit team identified $1.3 million in federal match money that was inappropriately drawn down from CMS."
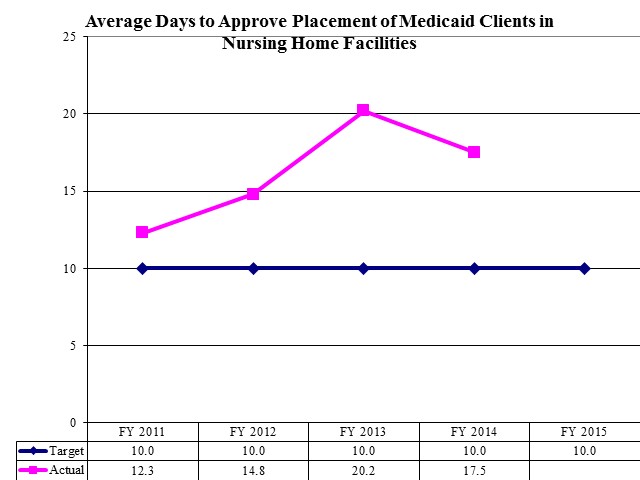
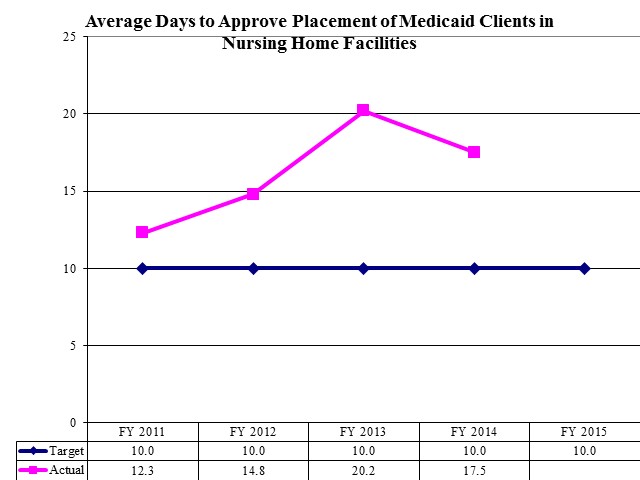
Average Days to Approve Placement of Medicaid Clients in Nursing Home Facilities
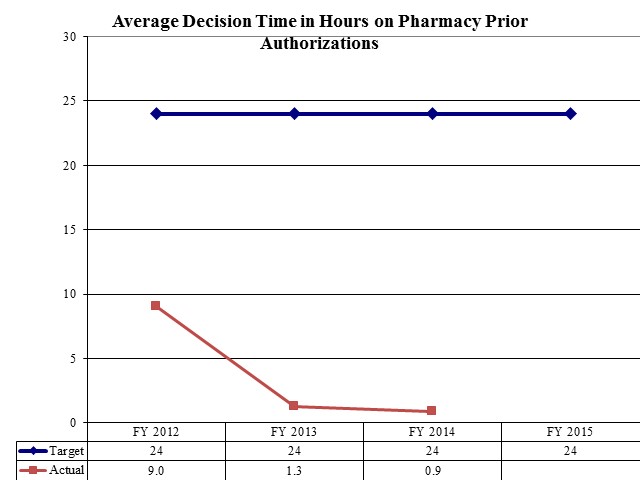
Average Decision Time in Hours on Pharmacy Prior Authorizations
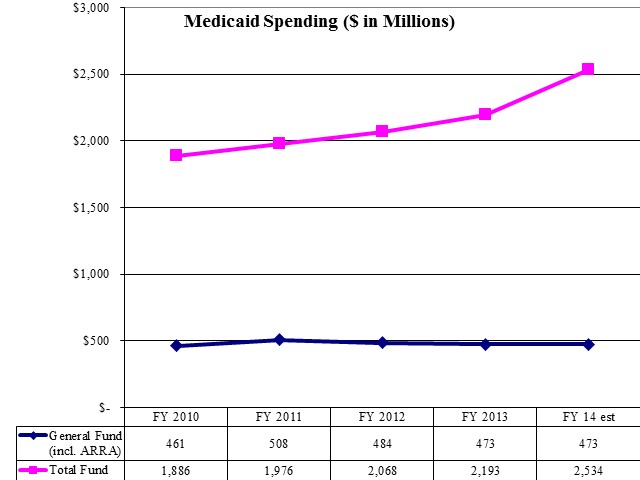
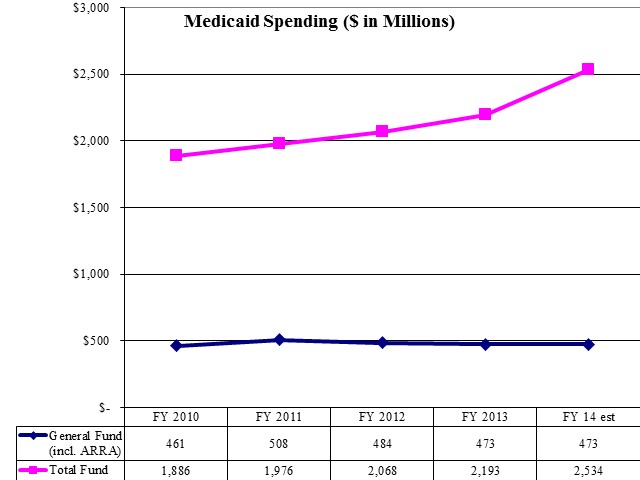
Medicaid Spending ($ in Millions)
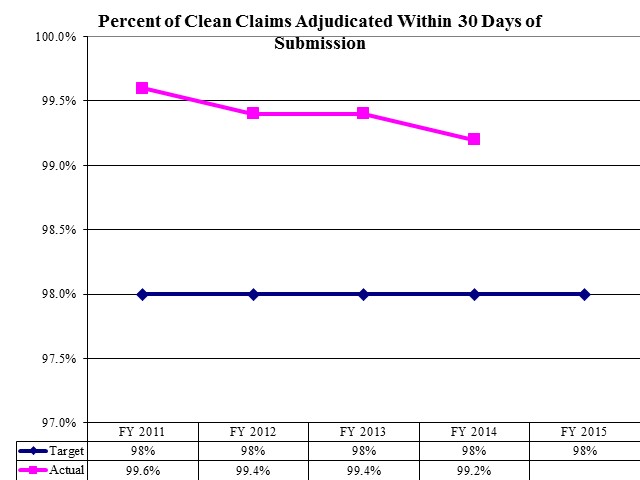
Percent of Clean Claims Adjudicated Within 30 Days of Submission
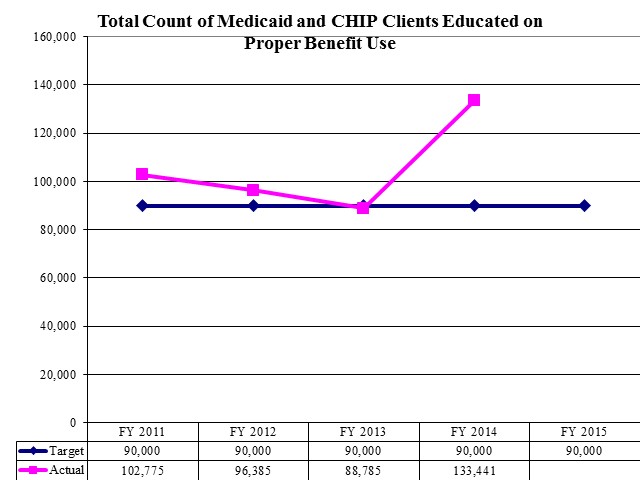
Total Count of Medicaid and CHIP Clients Educated on Proper Benefit Use
Federal regulations provide for a wide variety of funding ratios ranging from 50 to 90 percent for different classes of positions and functions for this Division. The Division includes the following seven offices or bureaus: Director's Office, Financial Services, Eligibility Policy, Coverage and Reimbursement, Medicaid Operations, Managed Health Care, and Authorization and Community Based Services. The Division also includes the following three budget programs: DWS Seeded Services, Other Seeded Services, and Contracts.
Federal law requires that the Medical Care Advisory Committee serve as an advisory board to the Division. This committee consists of providers, Medicaid recipients, representatives from the Department of Human Services and the Department of Workforce Services, and members of the community. The committee advises the Division on program content, policy, and priorities. The Committee is advisory and its decisions are not binding on the Division.
The Medicaid Fraud Control Unit's mission is: "To protect the integrity of the Medicaid program and the safety and property of institutionalized citizens of the State of Utah through skilled detection, proactive investigation, prevention, prosecution and financial recovery." The Unit operates in the Attorney General's Office and focuses on criminal and civil actions against fraudulent providers and perpetrators of neglect and abuse against vulnerable adults in care facilities.
For analysis of current budget requests and discussion of issues related to this budget click here.
COBI contains unaudited data as presented to the Legislature by state agencies at the time of publication. For audited financial data see the State of Utah's Comprehensive Annual Financial Reports.